Regional coordinators of Mental Health Services in Ghana have lamented the severe and persistent shortage of essential psychiatric medicines for mental health patients in the country in the whole of 2015.
The shortage, they reported, had in many ways affected mental health care delivery of the already lackadaisically supported Mental Health Services of the Ghana Health Service (GHS).
To this end, patients and facilities had no option than to resort to the open market where prices of such medications were very expensive.
The situation also forced most patients and their caregivers to refuse review visits since they could not afford their medications and in some cases not get it at all.
These revelations came out when the regional coordinators took turns to present their 2015 review reports at the recently held 2016 annual performance review of the Mental Health Service in Ghana.
The review meeting which was held at Hotel Stevens in Ho brought together representatives from the World Health Organisation (WHO), Ghana, Ministry of Health (MoH), Ghana Health Service (GHS), Ghana Psychology Council, Ghana Psychic & Traditional Healing Association, Regional House of Chiefs as well other stakeholders participating for the first time. It was under the theme: ‘Consolidating The New Era of Mental Health in Ghana’.
The acute shortage was also confirmed by the Mental Health Authority (MHA) when the Chief Executive Officer (CEO), Dr Akwasi Osei, presented a review report of the authority.
. He acknowledged that inadequate supply of psychotropic medicines nationwide, including regional and community levels was a major challenge of the authority in ensuring quality mental health care delivery.
The discussions at the review meeting indicated that the shortage was mainly due to the lack of funds which was not forthcoming from the government and some bureaucratic procurement processes.
Dr Osei, therefore, assured that the authority was working on the Legislative Instrument (LI) for Mental Health Act 846, with a passing expected later in the year. More so, plans are far advanced to ensure that the Mental Health Fund (MHF) is well managed to support care.
Key directors would also be appointed to coordinate the various aspects of mental health care delivery, including the efficient supply of medicines.
That aside, the board of the MHA would ensure enhanced and persistent engagement with pharmaceutical companies for local manufacture of some psychiatric medicines otherwise known as psychotropics.
The annual mental health review meeting is to help mental health services providers, partners and stakeholders to look at how the sector fared in the previous year, with the view to mapping out strategies to improve the situation in the ensuing year.
Health News of Saturday, 27 February 2016
Source: kasapafmonline
No medicines for mental health patients
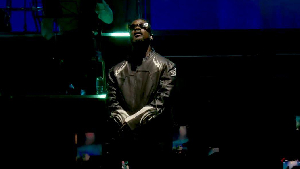
Entertainment